Venigalla B. Rao, Sunil Suhas Solomon win NIDA Avant-Garde Awards
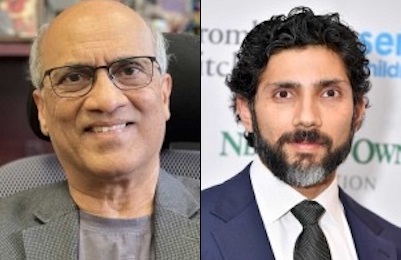
NIDA Avant-Garde Awards winners Venigalla B. Rao (left) and Sunil Suhas Solomon.
Indian American professors get National Institute on Drug Abuse’s awards for HIV and substance use disorder research
Two Indian American professors — Venigalla B. Rao and Sunil Suhas Solomon — are among the 2024 awardees of the National Institute on Drug Abuse’s (NIDA) Avant-Garde Award Program for HIV and Substance Use Disorder Research.
The program supports individual scientists of exceptional creativity at all career levels who propose high-impact research that will open new areas of HIV research and/or lead to new avenues for prevention and treatment of HIV among people who use drugs, according to a media release.
Rao, PhD, is a Professor of Biology and Founding Director of Bacteriophage Medical Research Center at The Catholic University of America, Washington, DC.
He obtained Ph D in Biochemistry from the Indian Institute of Science, Bangalore, India, and did post-doctoral research on bacteriophage T4 assembly and genome packaging at the University of Maryland Medical School.
He conducted seminal research to tease out the mechanisms of viral DNA packaging and established a multi-disciplinary research program to translate basic knowledge into vaccines and gene therapies against HIV and other infectious and genetic diseases.
Of particular significance is his current research to create new curative technologies interfacing bacteriophages and human cells. He received numerous research awards from National Institutes of Health and National Science Foundation, and holds 24 US and international patents. He is a Fellow of the American Academy of Microbiology, and a Fellow of the National Academy of Inventors.
His project, “Engineering Bacteriophage T4 as a Targeted Gene Therapy Drug for in vivo HIV Cure,” will establish a new category of in vivo HIV cure “drugs” that would potentially transform the health of substance users who are disproportionately affected by HIV disease, as well as that of ~39 million people across the globe who are living with HIV today, according to the release.
Using a novel large capacity bacteriophage T4 artificial viral vector technology developed in the Rao laboratory, nanoparticles will be programmed with a payload of genome editing molecules, which will target hematopoietic stem cells (HSCs) in vivo and introduce a delta-32 deletion mutation into the CCR5 HIV co-receptor gene.
The genetically modified HSCs will then differentiate and repopulate the body with HIV-resistant cells including CD4+ T cells which are now immune to HIV infection. These cells will replace the existing HIV reservoir resulting in a functional HIV cure.
Solomon, PhD , is a Professor of Medicine and Epidemiology in the Division of Infectious Diseases at the Johns Hopkins University School of Medicine. He completed his medical training in India and received an MPH and a PhD in Epidemiology from Johns Hopkins University. He has been elected to the Phi Beta Kappa and the Delta Omega honors societies.
His research is primarily focused on improving access to preventive and treatment services for HIV and viral hepatitis among vulnerable populations. He was one of the first recipients of the Avenir award (DP2) from NIDA. He served as the Protocol Chair of ACTGA5360 (MINMON), findings from which have impacted HCV guidelines globally.
In April 2019, he was awarded a $50 million co-operative agreement from PEPFAR/USAID to implement and evaluate innovative models of service delivery to improve the HIV care cascade in India with a focus on vulnerable populations.
He currently serves as the Co-Chair of the Substance Use Scientific Committee of the HIV Prevention Trials Network (HPTN) and the Protocol Chair of HPTN 103/PURPOSE4, the first trial of long-acting PrEP among PWID.
Solomon’s project is titled “Long-Acting Injectables for Treatment of HIV among PWID (LIFT HIV).” Long-acting antiretrovirals (LA ART) have the potential to revolutionize the delivery of HIV services; yet, there have been no data on the use of these agents among PWID including from low- and middle-income settings where viral suppression among PWID is several-fold lower than the general population.
The objective of Solomon’s project is to evaluate the feasibility and acceptability of LA ART via ethnography, estimate the efficacy and safety of LA ART vs. oral ART among previously unsupressed PWID via a clinical trial and model the cost-effectiveness of LA ART among PWID populations using agent-based modelling incorporating costs, according to the release.
